(Title image: Photo by Nik on Unsplash)
“I see pharmacological interventions in your future” is a paraphrasing of what my oncologist told me at my last doctor’s visit.
So let me back up a bit. I had my “eight-years-since-finishing-chemo” appointment with my oncologist last week. Things went the way they’ve been going for a while. He was very pleased with how things have been going and that made me feel very positive.
Certainly, I have my share of stressors churning at the moment, but most of them are not health-related. Most.
When my oncologist reviewed my bone density reports, however, he made the same prediction that he has during my previous two visits with him (see his quote above). The issue is that my bone scan in 2019 showed osteopenia, which I have to say is pretty weird given my lifestyle, which includes a lot of strength training. We both thought that perhaps it was an issue with the way the numbers were calculated.
Unfortunately, my 2024 bone scan showed a significant loss of bone compared to 2019. Enough to really concern my oncologist and befuddle us both.
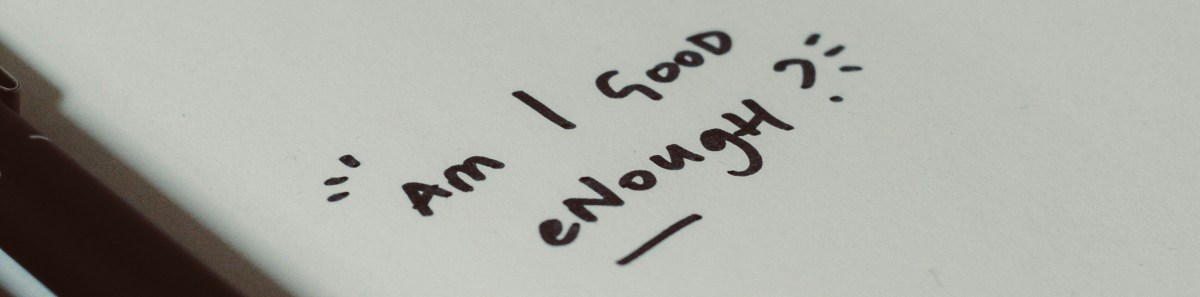
So despite my living the lifestyle that medical guidelines say I’m “supposed to” live in order to stay healthy and strong, it’s still not good enough.

(Photo by Mads Schmidt Rasmussen on Unsplash)
This harkens back to what I experienced after being diagnosed with breast cancer. It seemed like I had done everything I could to lessen my chances of getting cancer, including things that should have been protective, but there I was, a breast cancer patient, and a young one at that (which, I later learned, what one of the reasons the risk factors didn’t necessarily apply to me, but I didn’t know that at the time).
It drove my perfectionistic mind haywire.
It brought on feelings of helplessness and even despair.
The only thing that gave me a bit of a lift was learning to meditate. Meditation imparted a sense that I had a teensy bit of control, if not on the situation, at least in the way that I reacted to it.
I got through that period of my life, brushed myself off and went on. And for a while, I was feeling blessed.
But cancer treatments have long-term effects. And the repercussions of being pushed through menopause and being on endocrine therapy eventually caught up to me. Physical movements that used to be easy started to hurt. I lost muscle mass…and apparently, I lost bone too. I felt like I was treading water with a weight tied around me.
Never good enough.
So I am bearing down and reworking my diet and exercise program even more. And to be honest, this is also an opportunity to shed some of my perfectionistic tendencies. While I want to feel like I am doing everything I can to help stop my bone loss and avoid taking medication for it, I need to learn to give myself grace. Sometimes even doing everything “right” will not be 100% successful, and I have to be okay with that.

![Aging Muscle: After Cancer Treatment and Menopause [PHOTOS]](https://franticshanti.com/wp-content/uploads/2024/09/samuel-girven-bbr_zigemyq-unsplash_cropped.jpg?w=1200)












![“The Gun Show”: Assessing Biceps Muscle Loss Due To Endocrine Therapy [PHOTOS]](https://franticshanti.com/wp-content/uploads/2020/12/ambitious-creative-co-rick-barrett-uwk8is-hfj8-unsplash_cropped.jpg?w=1200)




