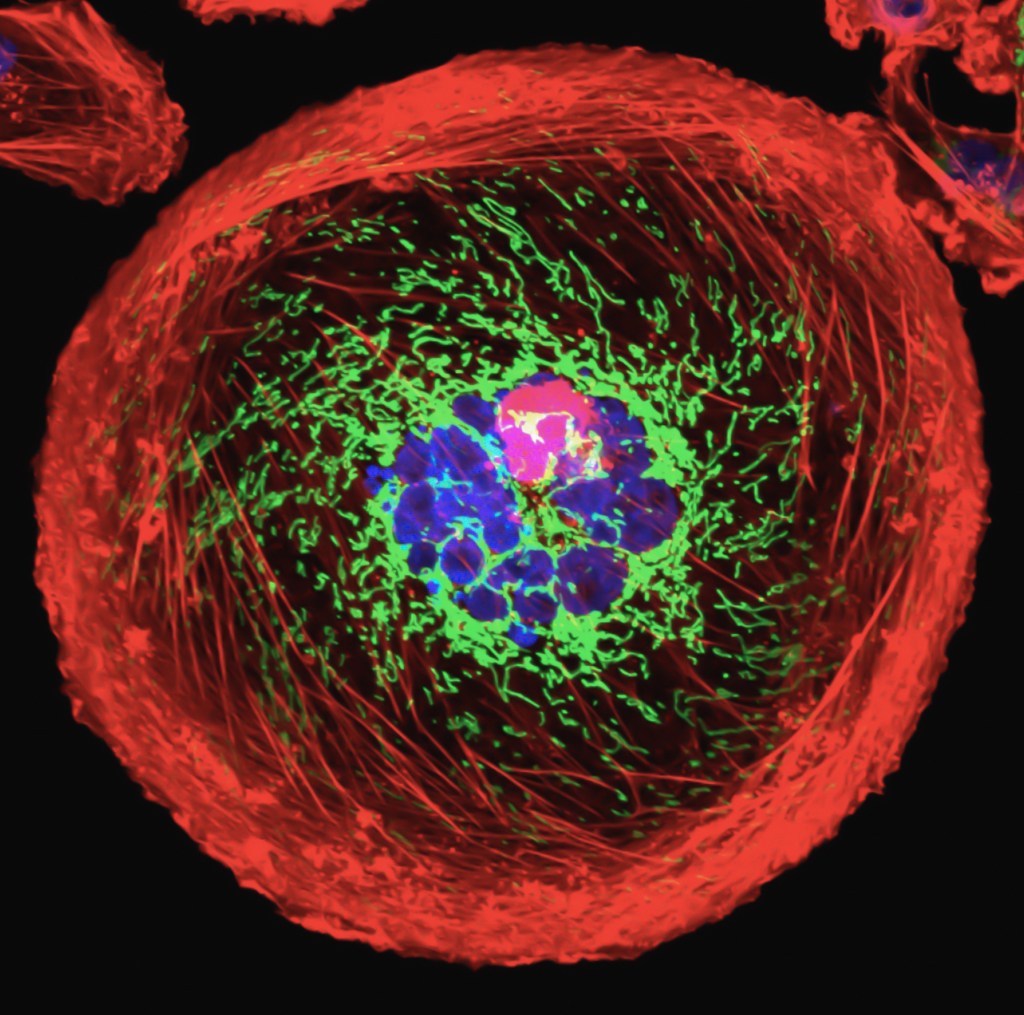
With as much sophisticated research as has been done on cancer, it still remains a confounding disease and much of the treatment may seem to be, for lack of a better word, medieval.
So it shouldn’t seem surprising that cancer patients also reach out for less conventional therapy to help themselves through the treatment process.
First, a clarification of terms used in this post:

- Conventional medicine: chemotherapy, radiation, surgery, immunotherapy, etc., prescribed by your medical team.
- Complementary medicine: non-standard treatment used in conjunction with conventional treatment; also called Integrative Medicine.
- Alternative medicine: non-standard treatment used instead of conventional treatment.
Therefore, generally speaking, what distinguishes complementary from alternative medicine is whether it’s used with standard medical treatment.
According to a study (Crudup et al., 2021) that was presented at the 2021 Annual Meeting of the American Society of Clinical Oncology (ASCO), 73% of breast cancer patient participants stated that they employed complementary therapies in their treatment. However, while oncologists were supportive of such therapies, they were not aware of the extent to which their patients utilized them and thought that only 43% of their patients did.

Furthermore, oncologists felt that counseling, support groups, exercise, etc. were the most effective non-standard therapies, in contrast to patients who found great benefit in meditation, mindfulness and spiritual practices. While two-thirds of both patients and oncologists felt that complementary medicine improved quality of life, a majority of patients also felt that it improved their outcomes.
Wayne Jonas, MD, a co-author of this study, says: “Cancer is a complex disease that affects every component of a patient’s life. While conventional medicine is effective for curing disease, it can fall short in helping patients heal. Patients are turning to these therapies to look for hope and to improve their quality of life and well-being after diagnosis… .”
What types of therapies do these include? The website “Cancer Health” provides examples of some complementary treatments (see here for an explanation of each):
Acupuncture
Aromatherapy
Art Therapy
Biofeedback
Cannabis
Herbal Therapies
Labyrinth Walking
Massage
Meditation
Music/Dance Therapy
Qigong
Spirituality
Tai Chi
Traditional Medicine (Ayurvedic, Chinese, etc.)
Vitamins and Supplements
Yoga
[This list is by no means exhaustive.]
I used a number of these complementary therapies myself and can attest to the important role they played in my recovery. As Dr. Jonas points out above, conventional treatments “can fall short in helping patients heal” [emphasis mine], whereas non-standard therapies seem to focus on that aspect.
I believe that these additional therapies, particularly more spiritual ones, are what give us hope throughout the cancer experience. Patients should be encouraged to seek out additional, complementary therapies to help themselves move through treatment, fully supported by their oncologists and ideally also guided by them.
Did you rely on complementary or alternative treatments to help you through your cancer journey?
~~~~~~~~~~~~~~~~~~~~~~~~~~~
REFERENCES
Original Research
Abstract for presentation:
Crudup et al. (2021) Awareness, perceptions, and usage of whole person integrative oncology practices: Similarities and differences between breast cancer patients and oncologists. Presented at 2021 Annual Meeting of the American Society of Clinical Oncology (ASCO), https://meetings.asco.org/abstracts-presentations/200685
Published research article:
Crudup et al. (2021) Breast cancer survivorship and level of institutional involvement utilizing integrative oncology. J Clin Oncol, 39, no. 15_suppl. e18588,
https://www.doi.org/10.1200/JCO.2021.39.15_suppl.e18588
Synopses
The ASCO Post Staff (June 7, 2021; updated June 15, 2021) Use of integrative medicine by patients with breast cancer. ASCO Post, https://ascopost.com/news/june-2021/use-of-integrative-medicine-by-patients-with-breast-cancer/
Tien C (June 28, 2021) Oncologists Underestimate the Number of Breast Cancer Patients Who Use Complementary Medicine. Cancer Health, https://www.cancerhealth.com/article/oncologists-underestimate-number-breast-cancer-patients-use-complementary-medicine
Descriptions of complementary therapies
Living with Cancer: Complementary Therapies. Cancer Health, https://www.cancerhealth.com/basics/health-basics/complementary-therapies